Varicocele is a common condition affecting men, particularly during puberty and adulthood. While it is widely associated with male infertility, its impact on testosterone levels has become a significant topic of discussion. Testosterone is the primary male hormone responsible for muscle growth, bone density, mood regulation, libido, and overall vitality.
Many men diagnosed with varicocele wonder: Can varicocele affect testosterone levels? The answer is not straightforward, as various factors influence testosterone production. However, emerging research suggests that untreated varicocele may contribute to lower testosterone levels, which can affect a man’s quality of life.
In this article, we will explore the link between varicocele and testosterone levels, the scientific mechanisms behind the condition, its symptoms, and potential treatment options. We will also discuss whether treating varicocele can restore testosterone production and improve overall health.
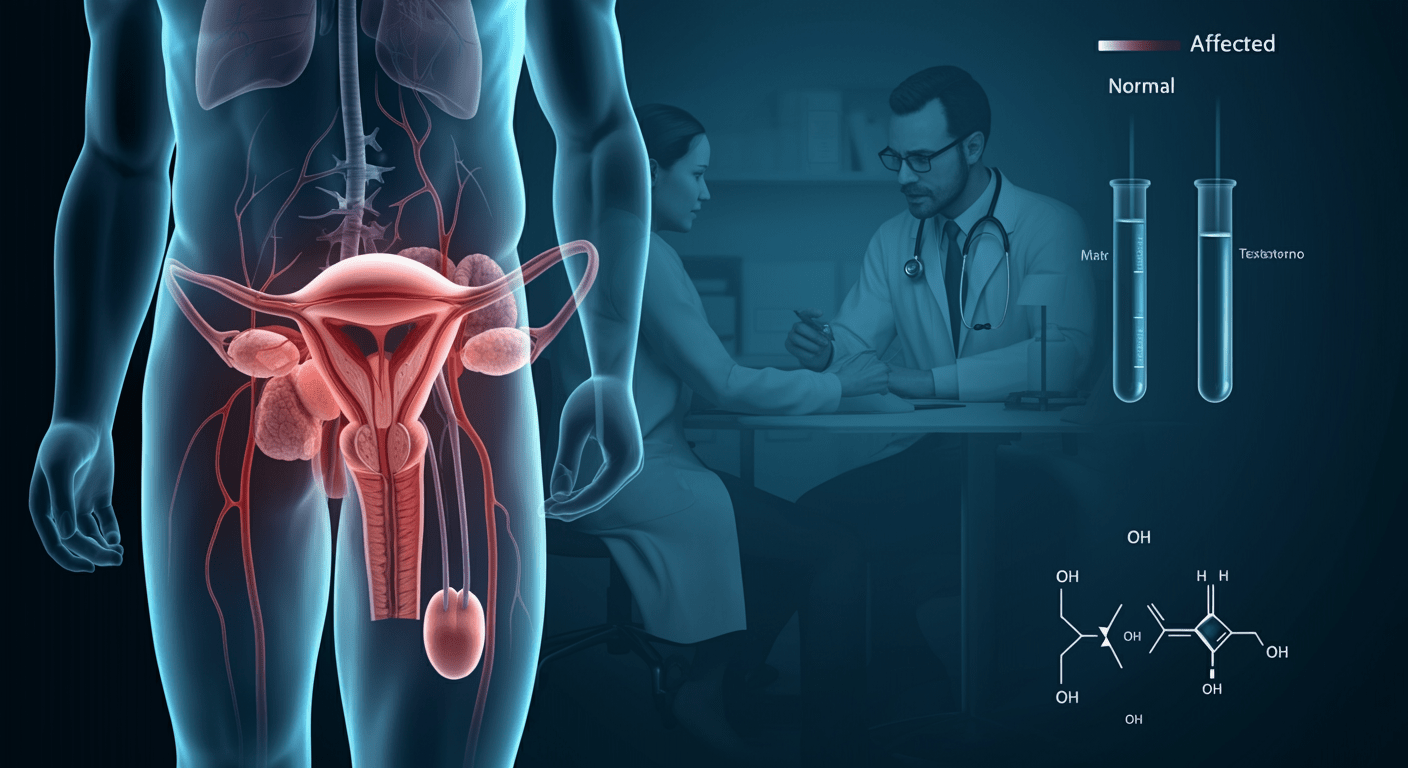
What is Varicocele?
A varicocele is an enlargement of the veins within the scrotum, similar to varicose veins in the legs. It occurs due to poor circulation, leading to blood pooling in the pampiniform plexus—a network of veins responsible for cooling the testicles.
Key Facts About Varicocele:
✔️ Affects 15% of adult males
✔️ More common on the left side due to anatomical differences
✔️ Present in up to 35% of men with primary infertility
✔️ May lead to reduced sperm quality and low testosterone production
While many men with varicocele remain asymptomatic, some experience discomfort, testicular shrinkage, infertility, or hormonal imbalances.
How Does Varicocele Affect Testosterone Production?
Testosterone is produced by Leydig cells in the testicles. A varicocele can interfere with this process due to several physiological factors:
1. Increased Scrotal Temperature
The pampiniform plexus acts as a cooling system, regulating testicular temperature. When a varicocele develops, this system becomes dysfunctional, causing excess heat accumulation in the testicles. Since testosterone synthesis requires an optimal temperature (~34°C or 93°F), prolonged heat exposure impairs Leydig cell function, leading to reduced testosterone production.
2. Oxidative Stress & Cellular Damage
Varicoceles can cause oxidative stress, where excess free radicals damage testicular tissues. This oxidative damage affects both sperm-producing Sertoli cells and testosterone-producing Leydig cells, leading to hormonal imbalances.
3. Blood Flow & Nutrient Deprivation
A varicocele disrupts normal blood circulation in the testicles, depriving them of essential oxygen and nutrients. As a result, the cells responsible for testosterone production struggle to function properly, leading to gradual testosterone decline.
Scientific Evidence Linking Varicocele to Low Testosterone
Several clinical studies have confirmed the link between varicocele and testosterone deficiency:
🔬 A study in the Journal of Urology found that men with varicoceles had lower testosterone levels than those without the condition. (Source)
🔬 Another study published in Fertility and Sterility reported that 70% of men who underwent varicocele repair experienced an increase in testosterone levels.
🔬 A meta-analysis in the National Institutes of Health (NIH) showed that varicocelectomy significantly improved testosterone production in men with clinically diagnosed varicoceles. (Source)
These findings suggest that varicocele not only affects sperm production but also has a direct impact on hormonal health.
Symptoms of Low Testosterone Due to Varicocele
Men with varicocele-related testosterone deficiency may experience the following symptoms:
✔️ Reduced Libido – Lower testosterone leads to decreased sex drive
✔️ Erectile Dysfunction – Difficulty achieving or maintaining erections
✔️ Fatigue & Low Energy – A lack of testosterone can cause constant tiredness
✔️ Depression & Mood Swings – Testosterone plays a role in emotional stability
✔️ Loss of Muscle Mass – Reduced testosterone leads to muscle weakness
✔️ Weight Gain & Increased Body Fat – Especially in the abdominal region
✔️ Decreased Bone Density – Increased risk of osteoporosis
If you experience these symptoms, consulting a specialist at Heal Life India can help determine if varicocele treatment is necessary to restore hormonal balance.
Can Treating Varicocele Restore Testosterone Levels?
Yes! Research has shown that treating a varicocele can significantly improve testosterone levels in affected men.
Varicocele Treatment Options
There are two primary medical interventions for varicocele:
1. Varicocelectomy (Surgical Repair)
✔️ Procedure: Ligation (cutting off) of abnormal veins to restore normal blood flow
✔️ Effectiveness: 70–80% success rate in boosting testosterone
✔️ Recovery Time: 2–4 weeks
✔️ Best for: Severe varicoceles causing infertility and hormonal imbalances
2. Varicocele Embolization (Minimally Invasive)
✔️ Procedure: A catheter is inserted into the vein, and a coil or blocking agent is used to close off abnormal veins
✔️ Effectiveness: High success rate, faster recovery than surgery
✔️ Recovery Time: 1–2 weeks
✔️ Best for: Mild to moderate varicoceles with hormonal symptoms
Lifestyle Changes to Support Testosterone Production
In addition to medical treatment, certain lifestyle modifications can help boost testosterone:
✔️ Exercise & Strength Training – Boosts testosterone naturally
✔️ Healthy Diet – Rich in zinc, vitamin D, and healthy fats
✔️ Adequate Sleep – 7-9 hours per night supports hormone balance
✔️ Stress Management – Chronic stress increases cortisol, which suppresses testosterone
At Heal Life India, we provide holistic treatment plans tailored to each individual, ensuring the best possible outcomes for men struggling with varicocele-related testosterone decline.
Frequently Asked Questions (FAQs) – Can Varicocele Affect Testosterone Levels?
Q. What causes varicocele?
A varicocele develops when the veins within the scrotum become enlarged due to faulty valves in the spermatic cord veins. Normally, these veins help regulate blood flow to and from the testicles, ensuring proper temperature control for sperm and testosterone production.
However, when these valves fail to function correctly, blood starts pooling in the veins, causing them to expand and form a varicocele. Over time, this leads to:
✔️ Increased scrotal temperature, which can negatively impact sperm and testosterone production
✔️ Reduced oxygen and nutrient supply to testicular tissues
✔️ Oxidative stress that damages Leydig cells responsible for testosterone production
While the exact cause of varicocele isn’t always clear, it is believed to be a result of genetic predisposition and anatomical factors. The condition commonly develops during puberty and is often found on the left side of the scrotum due to differences in venous drainage patterns.
Q. Can varicocele cause permanent testosterone loss?
Varicocele can lead to a long-term decline in testosterone production if left untreated. The severity of its impact depends on factors like:
✔️ How large the varicocele is (Grade 1, 2, or 3)
✔️ How long it remains untreated
✔️ Whether it causes testicular damage or shrinkage (atrophy)
✔️ The presence of symptoms like infertility or low testosterone levels
If a varicocele remains untreated for many years, it can cause:
❌ Progressive damage to the testicles
❌ Chronic oxidative stress leading to Leydig cell dysfunction
❌ Irreversible testosterone deficiency
However, early detection and treatment can prevent permanent damage. Many men experience a significant boost in testosterone levels after undergoing varicocele repair surgery (varicocelectomy) or embolization.
Q. How do I know if my varicocele is affecting my testosterone levels?
If varicocele is affecting testosterone production, you may experience several symptoms that indicate hormonal imbalance, including:
✔️ Reduced Libido (Sex Drive) – A sudden decrease in interest in sexual activities
✔️ Erectile Dysfunction – Difficulty achieving or maintaining an erection
✔️ Fatigue & Low Energy – Persistent tiredness, even after adequate rest
✔️ Mood Swings & Depression – Irritability, anxiety, or a general feeling of sadness
✔️ Loss of Muscle Mass – Weakness and difficulty in muscle building
✔️ Increased Body Fat – Especially around the abdominal area
✔️ Decreased Bone Density – Higher risk of fractures and osteoporosis
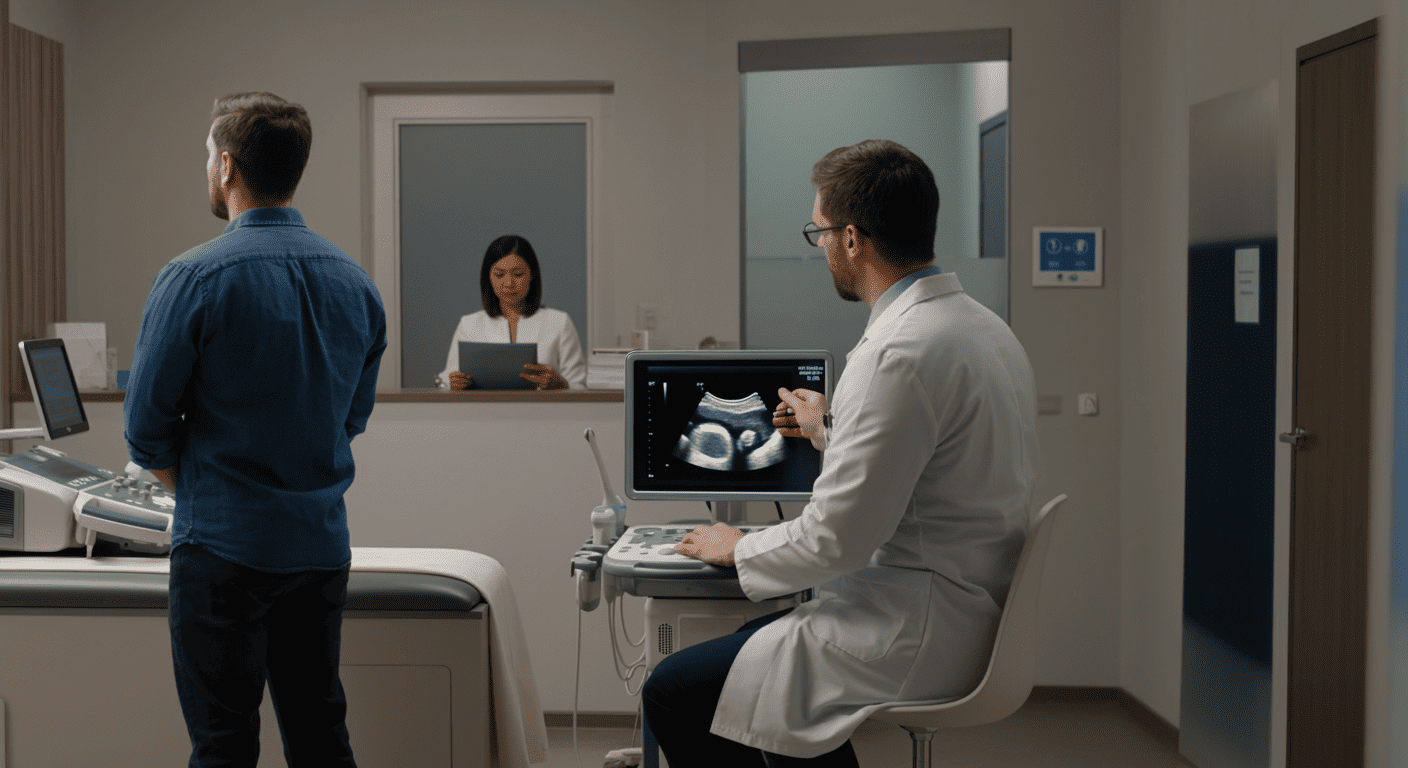
To confirm if varicocele is affecting testosterone, a doctor will recommend:
✅ A scrotal ultrasound – To evaluate varicocele size and severity
✅ A testosterone blood test – To check hormonal levels
✅ Semen analysis – To assess sperm health (if fertility concerns exist)
If your testosterone levels are below normal (300-1000 ng/dL) and you have varicocele, treatment may help restore hormonal balance.
Can all men with varicocele experience low testosterone?
No, not all men with varicocele experience a decline in testosterone levels. The impact of varicocele varies from person to person.
✔️ Some men with mild varicocele (Grade 1-2) may not experience any noticeable symptoms and maintain normal testosterone levels.
✔️ Others, especially those with Grade 3 varicocele, may experience hormonal imbalances and infertility.
Several factors influence whether a varicocele will cause low testosterone, including:
✅ Size of the varicocele – Larger varicoceles are more likely to affect testosterone
✅ Duration – Long-standing varicoceles may cause more damage
✅ Age – Older men with untreated varicoceles may experience a greater testosterone decline
✅ Overall health – Lifestyle, diet, and genetic factors play a role
Even if you do not have symptoms, it’s important to monitor your testosterone levels if you have a clinically significant varicocele.
Is surgery the only option for treating varicocele?
No, surgery is not the only treatment option for varicocele. The choice of treatment depends on varicocele severity, symptoms, and personal preference.
There are two primary medical interventions for varicocele:
1. Varicocelectomy (Surgical Repair)
✔️ Procedure: The affected veins are surgically tied off or removed to redirect blood flow
✔️ Effectiveness: 70-80% of men experience a testosterone increase after surgery
✔️ Recovery Time: 2-4 weeks
✔️ Best for: Severe varicoceles causing testicular pain, infertility, or low testosterone
2. Varicocele Embolization (Minimally Invasive)
✔️ Procedure: A small coil or blocking agent is inserted via a catheter to shut down abnormal veins
✔️ Effectiveness: Similar to varicocelectomy, with faster recovery
✔️ Recovery Time: 1-2 weeks
✔️ Best for: Mild-to-moderate varicoceles or patients seeking a non-surgical option
In some cases, if testosterone levels are not severely affected, lifestyle changes and regular monitoring may be sufficient. However, if testosterone deficiency is causing significant symptoms, varicocele treatment is recommended to restore hormonal balance.
Where can I get professional treatment for varicocele in India?
At Heal Life India, we offer comprehensive varicocele diagnosis and treatment by top urologists and andrologists.
✔️ Expert Consultation – Personalized treatment plans for varicocele-related testosterone issues
✔️ Advanced Diagnosis – Ultrasound, blood tests, and semen analysis for a complete evaluation
✔️ Surgical & Non-Surgical Treatment – Varicocelectomy and embolization options available
✔️ Hormonal Therapy & Lifestyle Guidance – To naturally boost testosterone levels post-treatment
💡 Why Choose Heal Life India?
🏥 State-of-the-art medical facilities
🎯 Proven success rates in testosterone recovery
📍 Multiple locations across India
📞 Book a consultation today! Call us at 9060259427 or visit Healifeindia.com for more details.