Varicocele is a common medical condition affecting males, particularly during adolescence and adulthood. It occurs due to the enlargement of the veins within the scrotum, similar to varicose veins in the legs. This condition is often linked to infertility, discomfort, and testicular atrophy.
If you’re wondering, What are the different grades of varicocele? or How are the grades of varicocele classified?, this in-depth guide by Heal Life India will provide you with everything you need to know.
What is a Varicocele?
A varicocele is a condition where veins inside the scrotum become enlarged due to faulty valves, which prevent proper blood flow. This results in blood pooling, leading to swelling and, in some cases, pain or fertility issues.
Varicoceles are classified into different grades based on their severity, visibility, and impact. Understanding these grades can help in determining the right treatment plan.
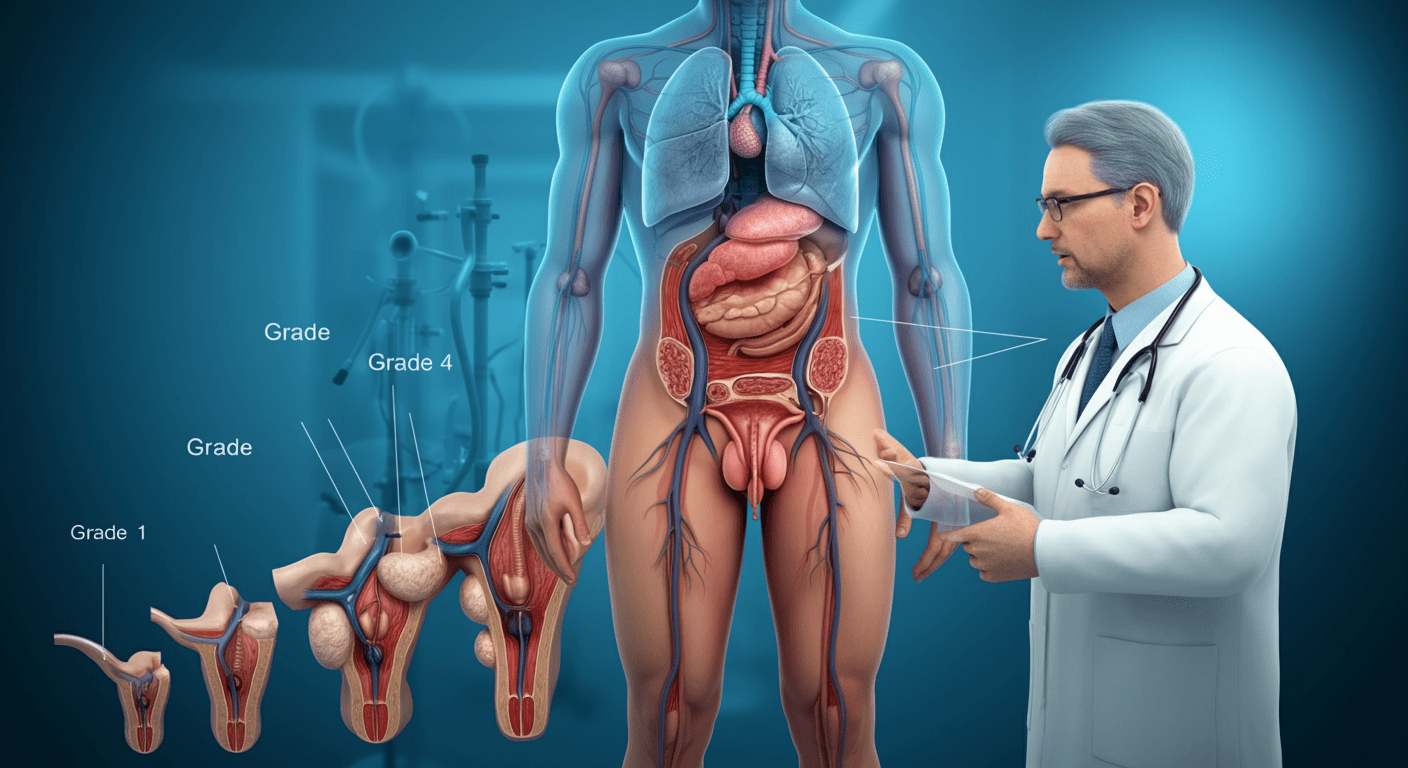
What Are the Different Grades of Varicocele?
Varicoceles are categorized into three primary grades based on physical examination findings. A more detailed grading system using ultrasound may also be used to further classify them.
Grade I Varicocele (Mild)
- Detection: Cannot be seen or felt under normal conditions.
- Diagnosis: Only detected when performing the Valsalva maneuver (a technique where the patient bears down to increase abdominal pressure, making the veins more prominent).
- Symptoms: Often asymptomatic but may cause mild discomfort.
👉 Significance: This is the least severe grade and rarely requires treatment unless it causes pain or affects fertility.
Grade II Varicocele (Moderate)
- Detection: Not visible but can be felt during a physical examination even without the Valsalva maneuver.
- Diagnosis: More noticeable than Grade I but still not easily seen.
- Symptoms: Can cause a dull aching sensation, particularly after standing for long periods or physical activity.
👉 Significance: This grade is more noticeable and may impact sperm production or cause mild discomfort.
Grade III Varicocele (Severe)
- Detection: Clearly visible through the scrotal skin and easily palpable.
- Diagnosis: No special maneuver is needed for detection.
- Symptoms: Often associated with testicular pain, atrophy (shrinking of the testicle), and potential fertility issues.
👉 Significance: This is the most severe form and often requires medical intervention if it leads to pain or infertility.
Advanced Grading System (Ultrasound-Based)
In addition to the three primary grades, Doppler ultrasound can be used to further classify varicoceles into five additional grades, according to the Sarteschi classification:
- Grade I: Blood reflux only at the groin level during the Valsalva maneuver.
- Grade II: Reflux is seen in the upper part of the pampiniform plexus (a network of veins in the spermatic cord).
- Grade III: Reflux extends to the lower scrotum only during the Valsalva maneuver.
- Grade IV: Continuous reflux in the scrotal veins, causing deformation and possible testicular shrinkage.
- Grade V: Severe, resting reflux in dilated veins, often with testicular atrophy.
These additional classifications help determine the severity of venous reflux and guide treatment decisions.
How Is Varicocele Diagnosed?
A varicocele is typically diagnosed through a physical examination by a urologist. However, if the varicocele is not easily detected, a scrotal ultrasound may be used to assess vein dilation and blood flow.
Diagnostic Methods:
- Physical Examination: Identifies varicoceles through palpation.
- Valsalva Maneuver: Helps detect smaller varicoceles.
- Doppler Ultrasound: Confirms the diagnosis and determines the severity.
- Semen Analysis: Assesses sperm quality, especially if infertility is a concern.
What Are the Symptoms of a Varicocele?
Most varicoceles are asymptomatic, but when symptoms occur, they may include:
✔ Scrotal pain or discomfort – A dull ache that worsens with prolonged standing.
✔ Heaviness in the scrotum – A dragging sensation due to blood pooling.
✔ Visible enlargement of veins – More prominent in severe cases.
✔ Testicular atrophy – Shrinking of the affected testicle.
✔ Infertility – Associated with reduced sperm count and motility.
If you experience these symptoms, it’s important to seek medical advice from Heal Life India, where expert specialists can guide you.
What Are the Treatment Options for Varicocele?
The treatment approach depends on the severity of the varicocele and its symptoms.
Non-Surgical Treatment (For Mild Cases)
- Observation: If there are no symptoms or fertility concerns, no treatment is required.
- Pain Management: Over-the-counter pain relievers such as ibuprofen or acetaminophen.
- Supportive Care: Wearing scrotal support or compression underwear can help relieve discomfort.
Surgical Treatment (For Severe Cases)
If the varicocele causes pain, testicular atrophy, or infertility, surgery may be recommended.
1. Varicocelectomy (Open Surgery)
- Involves tying off the affected veins to redirect blood flow.
- Performed under general anesthesia.
- High success rate for fertility improvement.
2. Laparoscopic Varicocelectomy
- A minimally invasive technique using small incisions and a camera.
- Faster recovery time compared to open surgery.
3. Percutaneous Embolization
- A non-surgical procedure where a coil or sclerosing agent is placed in the veins to block abnormal blood flow.
- Done under local anesthesia.
- Lower risk of complications but not as commonly performed as surgery.
Frequently Asked Questions (FAQs)
What is the main cause of a varicocele?
A varicocele occurs when the valves inside the testicular veins malfunction, leading to poor blood circulation in the scrotum. These veins are responsible for draining blood from the testicles back to the heart. When the valves fail, blood pools in the veins, causing them to enlarge.
Several factors contribute to varicocele formation:
Genetics: A family history of varicoceles or varicose veins increases the risk.
Increased Abdominal Pressure: Straining due to heavy lifting, chronic constipation, or prolonged standing can lead to varicoceles.
Anatomical Factors: The left testicular vein is longer and enters the left renal vein at a right angle, which makes it more prone to developing varicocele.
While the exact cause remains unknown, these factors increase the likelihood of developing varicoceles.
Can a varicocele go away on its own?
No, varicoceles do not go away on their own. Once the veins become enlarged, they do not shrink or return to normal size without treatment. However, the severity and symptoms of a varicocele may remain stable or worsen over time.
For mild varicoceles (Grade I or II), treatment is not always necessary unless they cause:
Pain
Testicular shrinkage
Infertility issues
If symptoms persist or worsen, Heal Life India recommends consulting a urologist to discuss treatment options.
Is varicocele surgery necessary for all cases?
No, surgery is not always required. The need for surgery depends on:
Severity of symptoms (pain, testicular atrophy, infertility)
Grade of varicocele (higher grades are more likely to need treatment)
Fertility concerns (if sperm quality is affected)
When is varicocele surgery recommended?
Painful Varicocele: If the patient experiences persistent discomfort that interferes with daily activities.
Infertility Issues: If the varicocele is affecting sperm count, motility, or morphology.
Testicular Atrophy: If the affected testicle has shrunk due to poor blood circulation.
Failure of Conservative Treatment: If pain persists despite lifestyle modifications and pain management.
At Heal Life India, our specialists can assess your condition and recommend the best course of action.
How long does varicocele surgery recovery take?
Recovery time depends on the type of surgical procedure performed.
Open Varicocelectomy (Microsurgery)
Hospital Stay: Same-day discharge (outpatient procedure)
Recovery Time: 2-4 weeks
Post-Surgery Care: Avoid strenuous activity for at least 2 weeks.
Laparoscopic Varicocelectomy
Hospital Stay: Same-day discharge
Recovery Time: 1-2 weeks
Post-Surgery Care: Minimal activity restriction.
Percutaneous Embolization (Minimally Invasive)
Hospital Stay: Same-day discharge
Recovery Time: 1-2 days
Post-Surgery Care: Resume normal activities quickly.
At Heal Life India, we provide minimally invasive surgical options to ensure a quick and smooth recovery.
Can varicocele lead to erectile dysfunction (ED)?
No, varicocele itself does not directly cause erectile dysfunction. However, it may lead to low testosterone levels, which can indirectly affect libido and sexual function.
How does varicocele affect testosterone?
Poor blood circulation in the testicles increases scrotal temperature.
Testosterone production is sensitive to temperature changes.
Over time, this may lead to low testosterone levels, affecting energy levels, mood, and libido.
If you experience symptoms of low testosterone, Heal Life India can evaluate and provide appropriate treatment.